
Prolapse After Giving Birth: Everything You Need to Know

New mamas know that a lot of things happen to the body before, during, and after pregnancy. There’s the expected — weight gain, skin changes, hair loss. And then there’s the unexpected. Although it’s rarely discussed, pelvic organ prolapse is a shockingly common post-childbirth complication that many women don’t anticipate. In this guide, we’re going over everything you need to know about this condition so you can handle it with confidence.
Defining Pelvic Organ Prolapse
Let’s start with the basics. What is pelvic organ prolapse? “Prolapse is a loss of the supportive function of our pelvis,” says Doctor of Physical Therapy Heather Jeffcoat, owner of Fusion Wellness. “This goes beyond just muscle defects and includes loss of integrity of connective tissue, fascia, and ligaments.” In other words, prolapse occurs when the tissues and muscles of the pelvic floor lose support and allow the organs to drop from their proper position.
What are the signs of prolapsed bladder or uterus you might ask? The reality is that many women are entirely asymptomatic and don’t even realize prolapse has occurred. “Other times, they report things like vaginal heaviness, urinary or fecal incontinence, difficulty emptying their bladder or bowels, and feeling like something is falling out of their vagina or feeling like they are sitting on a ball,” says Dr. Rachel Gelman, owner of Pelvic Wellness & Physical Therapy in San Francisco.
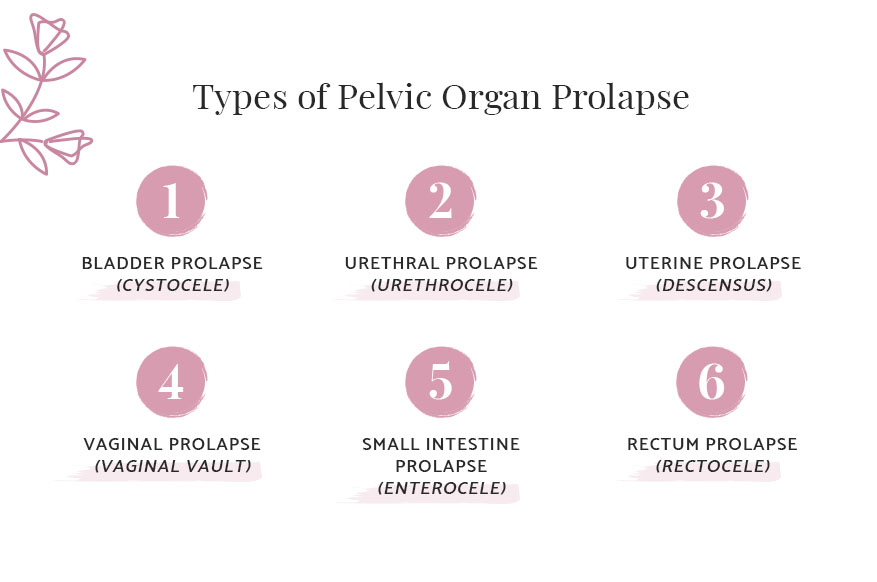
Types of Pelvic Organ Prolapse
Bladder Prolapse (Cystocele)
Urethral Prolapse (Urethrocele)
Uterine Prolapse (Descensus)
Vaginal Prolapse (Vaginal Vault)
Rectum Prolapse (Rectocele)
Small Intestine Prolapse (Enterocele)
How Common Is Prolapse After Giving Birth?
How common is it, exactly? “It depends on the research you look at, but one study shows that after one vaginal delivery, a quarter to half of the women demonstrate a mild prolapse during the first postpartum year,” says Dr. Gelman. It’s important to note that while vaginal delivery is a huge contributor, other factors can lead to a prolapse as well, including chronic constipation, menopause, heavy lifting, and obesity.
Why Prolapse Happens After Giving Birth
Many things happen during pregnancy that can take a toll on the body, especially in the pelvic region. In essence, prolapse happens due to injury sustained by the pelvic floor during vaginal delivery. “The pelvic floor stretches up to 245 percent of its original size during an uncomplicated, unassisted vaginal delivery,” says Dr. Jeffcoat. “When forceps or vacuum-assistance is performed, there is a quicker stretch of these muscles, increasing their chance of injury.”

Does C-Section Prevent Prolapse?
So, with that in mind, does having a Cesarean delivery (C-section) prevent organ prolapse? Unfortunately, no. Pelvic floor dysfunction increases during pregnancy regardless of the mode of delivery. However, women who have a C-section do have a lower risk of developing pelvic organ prolapse, says Dr. Jeffcoat.
What Is Pelvic Floor Dysfunction?Treating Post-Childbirth Organ Prolapse
Luckily, if your organs prolapse after childbirth, it does not necessarily mean you’ll have to experience this discomfort forever. In fact, there are some highly effective treatment options that can make the condition more bearable, from doing simple pelvic floor exercises to undergoing routine surgery. Before outlining a treatment plan, your doctor will determine the stage of prolapse, often using the Pelvic Organ Prolapse Quantification (POP-Q) system.
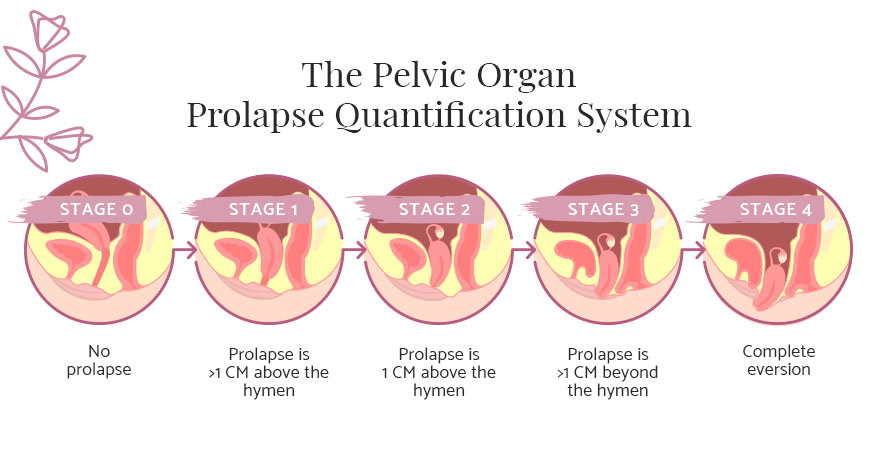
Stage 0: None
Stage 1: Prolapse Is >1 CM Above the Hymen
Stage 2: Prolapse Is 1 CM Above or Beyond the Hymen
Stage 3: Prolapse Is >1 CM Beyond the Hymen
Stage 4: Complete Eversion
Pelvic Floor Physical Therapy
Effective yet relatively conservative, pelvic floor physical therapy can help you strengthen the muscles in the pelvic floor so they can lift and support the pelvic organs. What is pelvic floor therapy? Your physical therapist may encourage you to perform pelvic floor exercises — such as doing Kegels — both at home and in a clinical setting. While using Kegel balls can certainly work, they should be part of a broader treatment plan.
Shop All Kegel Balls from Sofia & Grace“An internal examination by a skilled pelvic floor physical therapist is critical to determine if muscle overactivity, underactivity, or a combination of these two is present so that a custom treatment plan can be developed,” says Dr. Jeffcoat. “Kegels are not usually the answer — to tell a woman that she just needs to do kegels is oversimplifying a complex musculoskeletal presentation of symptoms.”
In actuality, most women suffering from postpartum prolapse require a combination of manual internal muscle techniques as well as strength and coordination treatments of the specific muscles in the pelvic floor.
Pessary
Another relatively conservative option for treating postpartum prolapse is the pessary. Essentially, a pessary is a silicone device that’s inserted into the vagina to help hold up the muscles and create support. Pessaries are flexible silicone devices that are positioned at the top of the vagina similar to a diaphragm.
Surgery
Surgery to correct organ prolapse is surprisingly common, and for good reason. Though it’s the most invasive, this form of intervention is highly effective and has excellent outcomes for many patients. But surgery isn’t right for all patients. It should be reserved for women who are done having kids — this is because pregnancy increases risk of prolapse, and surgery will not prevent it from happening again — and those who have more advanced stages of prolapse.
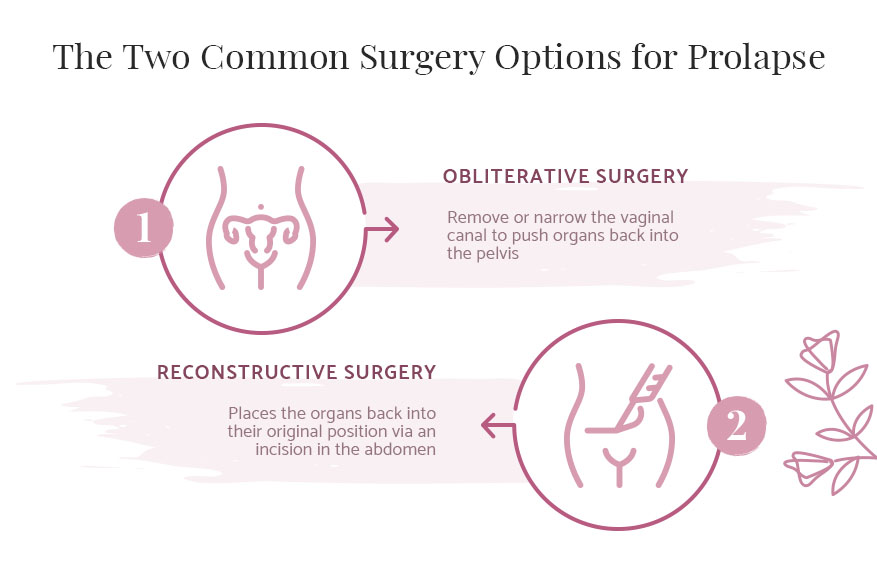
There are two common surgery options for prolapse:
- Obliterative surgery to remove or narrow the vaginal canal in order to push the organs back into the pelvis.
- Reconstructive surgery which physically places the organs back into their original position via an incision in the abdomen.
It’s important to note that surgery is not an alternative to pelvic floor physical therapy, and most patients must do both, says Dr. Jeffcoat. “Pelvic floor physical therapy is still required whether they decide to have surgery or not, as there is often loss of strength and coordination of pelvic floor muscles and muscles accessory to the pelvic floor, such as the gluteal muscles.”
Learn More About Pelvic Floor Therapy HereWe’re Here to Help
Pregnancy and childbirth are incredible physical feats. Experiencing prolapse — or any other physical response to pregnancy, for that matter — doesn’t mean you’re weak or out of shape. Sofia & Grace is here to help you find answers and address common problems so you can enter every stage of life with confidence and ease, whether it be motherhood or menopause.
Image Credits
Natalia Deriabina/shutterstock.com
Troyan/shutterstock.com
Maji Design/shutterstock.com
rumruay/shutterstock.com
nanmulti/shutterstock.com