
11 Helpful Hysterectomy Recovery Tips for Safe Healing

A hysterectomy is a procedure that removes the uterus, or womb, from the body. The uterus is the organ that grows the baby when a woman is pregnant. Removing the uterus means that you will stop having menstrual periods and will be unable to become pregnant. Sometimes, the ovaries and fallopian tubes may also be removed during the surgery. If the ovaries are removed, then you will enter menopause no matter how young or old you are.
Below, we cover what you need to know about different types of hysterectomies and then offer the best hysterectomy recovery tips for safe healing.
Reasons to Get a Hysterectomy
There are many different reasons that your doctor might recommend a hysterectomy as a course of treatment. During an interview with a woman in our community, she said the reason for her hysterectomy was due to menstruation difficulties. Other reasons to consider a hysterectomy include:
- Cancer in the uterus, cervix, and/or ovaries
- Endometriosis
- Abnormal vaginal bleeding
- Uterine fibroids that cause pain, bleeding, and other symptoms
- Uterine prolapse, or a sliding or movement of the uterus
- Chronic pelvic pain
- Adenomyosis, or a thickening of the uterus
In most cases except cancer, a doctor will recommend a hysterectomy only as a last resort if all other treatments have failed. While a hysterectomy is a relatively routine surgery and most people recover without issue, there are some risks to be aware of, including some that are common to pretty much any surgery. Some risks that you should be aware of include:
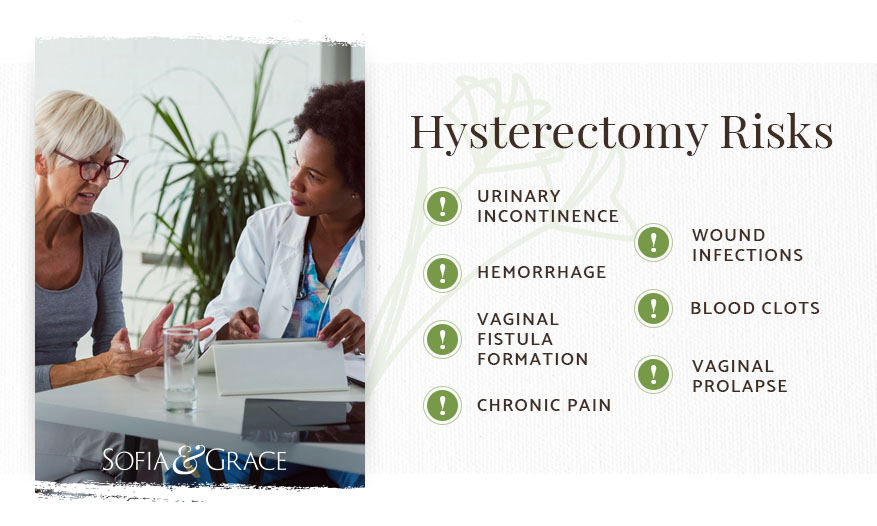
- Urinary incontinence
- Vaginal prolapse
- Vaginal fistula formation
- Chronic pain
- Wound infections
- Blood clots
- Hemorrhage
What are the types of hysterectomies?
There are many different types of hysterectomies, and it’s important to know which type you are undergoing and what exactly will be removed during the surgery. The types of hysterectomies and related surgeries are:
- Supracervical or subtotal hysterectomy: only the upper part of the uterus is removed, while the cervix is left in place
- Total hysterectomy: both the uterus and cervix are removed
- Radical hysterectomy: the uterus and cervix are removed in addition to tissue along the sides of the uterus and the top part of the vagina; this type of surgery is typically only used in the case of cancer
- Oophorectomy: removal of the ovaries
- Salpingectomy: removal of the fallopian tubes
- Hysterectomy and bilateral salpingectomy-oophorectomy: removal of the uterus, both ovaries, and both fallopian tubes
Your surgeon might also employ several different techniques to accomplish the hysterectomy. The main categories are open surgery and minimally invasive procedures.

Open surgery
An abdominal hysterectomy is the most common hysterectomy surgical technique, with more than half of all hysterectomies being performed this way. In an abdominal hysterectomy, a surgeon makes a five- to seven-inch long incision in the stomach. The incision may be horizontal or vertical. The uterus is removed through this incision. An abdominal hysterectomy usually requires a two- to three-day hospital stay and will also result in a visible scar once healing has finished. Total recovery time usually takes four to six weeks.
Minimally invasive procedures
Not all surgical procedures require a large incision, and some of the other hysterectomy options are less invasive. The minimally invasive procedures that you should be familiar with are:
- Vaginal hysterectomy: the uterus is removed through an incision in the vagina; this approach leaves no visible scar
- Laparoscopic hysterectomy: the surgery is performed with the aid of a laparoscope, or lighted camera; the laparoscope and surgical tools are inserted through small incisions made in the stomach
- Laparoscopic-assisted vaginal hysterectomy: the uterus is removed through the vagina using the aid of a laparoscope; usually one incision is made in the belly (for the camera) and the other is made in the vagina (to remove the uterus)
- Robot-assisted laparoscopic hysterectomy: the uterus is removed in a way similar to a laparoscopic hysterectomy, except the tools are part of a sophisticated robotic system that the surgeon can control from outside the body
Minimally invasive procedures offer many benefits, including shorter hospital stays, reduced pain and scarring, less risk of incisional hernias, a reduced chance of infection, and faster recovery time (usually in the range of two to three weeks, as opposed to four to six weeks). Costs are also usually lower for minimally invasive procedures, although robot-assisted surgery can get quite expensive.
However, not everyone is a good candidate for minimally invasive surgeries. The size of the uterus, scar tissue from previous surgeries, obesity, and your health status all affect whether or not you’d be a good candidate for a less invasive surgery. Talk to your doctor about your surgical options if you’d like a minimally invasive procedure.

Hysterectomy Recovery Tips
Here’s what you need to know about recovering from a hysterectomy:
Rest up as much as you can.
While a hysterectomy is very common, it’s also a surgical procedure, and your body needs time to recover accordingly. In the days and weeks following the surgery, you may find yourself much more tired than usual. This is totally normal, as your body needs rest to recover from a surgical procedure and going under anesthesia often results in lingering exhaustion. Sleep as much as you can and rest whenever your body tells you to. The more you sleep, the easier and faster your recovery will be, so don’t push your body too hard.
Take care of your incision site.
Follow your medical team’s instructions for taking care of your incision site. These instructions will vary depending on whether you have a vaginal incision or abdominal incision. Keeping the incision clean, dry, and sterile is important to stave off infection. If you have tape on the incision site, leave it on until it falls off, which should take about a week. The stitches will dissolve on their own. If the wound leaks or rubs against clothing, cover it in gauze and change the dressing at least once a day. If you have vaginal discharge or urine leakage, then many incontinence products for women can help keep you dry and comfortable while you wait to heal up.
Shop All Bladder Control Products for Leakage Protection
Manage your pain.
Just as with any surgery, you may experience significant soreness and pain after your surgery. Take your pain medication as prescribed — make sure not to take too much too soon, but also don’t wait to take the medication until you’re in severe pain. Medication takes time to set in, and sometimes it builds in your system, so you should follow the instructions even if you feel okay in the moment. By controlling the infections and pain, the medications will help get the healing process underway and help you rest comfortably. If you experience any side effects of the medications prescribed, talk to your doctor about getting switched to a different type of drug.
Eat the right diet.
Having a hysterectomy can affect your bowel movements, and it’s actually pretty common to be constipated for three to four days after surgery. To help ease constipation, it’s recommended that you eat lots of fruits, vegetables, and whole grains, which are high in nutrients as well as fiber and thus will promote regular bowel movements. Drink plenty of water, which will help soften your stools and make it easier to go to the bathroom. If you still haven’t been able to go after four days, then try taking a stool softener or a laxative, which will make it easier to get everything out of your system and also reduce strain on the area during defecating.
Menopause and Bloating: 4 Ways to Find Relief
Wear loose, soft clothing.
When you’re recovering from surgery, you want to wear loose, breathable clothing that won’t trap sweat and bacteria around the incision site. Loose shirts, big pants, and dresses or tunics are all good options. Be sure to prioritize soft fabric that won’t scratch or irritate your skin. Avoid pants that have a waistband that hits over your incision site. You don’t want any chafing in that area especially. Feeling comfortable is much more important than looking good in that period following surgery.
Hit pause on your love life.
You’ll need to take a temporary break from sex while your body heals up from surgery. Basically, you need to leave your vagina and the surrounding area alone while it heals (this also means no tampon use and no douching). Don’t have sex until the doctor clears you for it, or you could further injure the area and prolong your recovery.
Avoid strenuous tasks and activities.
Just as with any surgery, you should avoid strenuous activities that could strain your body or infect the surgery site. Lifting heavy objects is a major thing to avoid, as is swimming or getting in a hot tub (the water can introduce bacteria and other germs into the wound). You’ll also need to avoid driving for the first few weeks, as the painkillers can make you too sleepy to operate a vehicle. Driving also requires full range of motion and the ability to twist fully around, which might not be possible without pain in the first few weeks after surgery. Get someone else to drive you and enjoy being chauffeured around.

Exercise, but gently.
Your doctor may recommend some light walking in the first few weeks after surgery. Walking helps get your blood flowing, which in turn reduces blood clots, and it can also help promote bowel movements and ease constipation. Walking will also help you slowly build your stamina to resume other types of exercises. However, you should avoid strenuous exercise such as weight lifting and plyometrics until your doctor clears you. This can take anywhere between three and six weeks, depending on what type of surgery you had. After you fully recover, your doctor may else recommend post hysterectomy exercises to strengthen the area. Additionally, your doctor may suggest purchasing Kegel balls and performing Kegel ball exercises later on in the recovery process.
Browse Our Kegel Ball and Accessories Collection
Prepare for the hormone surges.
If your ovaries are removed alongside your uterus, then you will immediately enter menopause and experience all of its side effects, including hot flashes, mood swings, vaginal dryness, difficult sleeping, and more — on top of recovering from the surgery. Talk to your doctor about what to expect and how to get menopause relief for your symptoms. They may recommend that you consider hormone replacement therapy to help ease your menopause symptoms.
Ask others for help.
In the first weeks after your surgery, you will need help with some basic tasks, including driving or lifting heavy objects. Getting a hysterectomy can also be a very emotional experience. Some women are relieved that their physical pain will finally be gone, while others mourn the fact that they will no longer be able to have children. Don’t be afraid to reach out to others for help, whether you need someone to drive you somewhere, a friend to chat with, or even a therapist to talk to. You shouldn’t have to recover from a hysterectomy alone!

Call your doctor if you are concerned.
Finally, if you start feeling worse, then you need to call your doctor for immediate medical care. Some emergency situations include:
- Pain that does not improve with medication
- Inability to pass stools or gas
- Vaginal discharge increases in volume or smells bad
- Upset stomach keeps you from drinking fluids
- Stitches become loose and/or blood soaks through the bandage
- Signs of infection (i.e., swelling, warmth, red streaks, pus, a fever)
- Vaginal bleeding requires pads to be changed more than once an hour
- Large clots discharged vaginally
- Signs of a blood clot in your lower body (pain, redness, and swelling in the area)
A hysterectomy is a relatively routine surgery, but that doesn’t mean that you shouldn’t take your recovery seriously. Follow these hysterectomy recovery tips to start feeling better soon. To learn more about other women’s health topics, including what pelvic floor therapy is, be sure to check out the rest of our resource center.
Image Credits
Zephyr_p/shutterstock.com
Lordn/shutterstock.com
KucherAV/shutterstock.com
Jacek Chabraszewsk/shutterstock.com
wavebreakmedia/shutterstock.com
PK289/shutterstock.com
Liderina/shutterstock.com
Microgen/shutterstock.com