
5 Best Exercises for Interstitial Cystitis

Also known as painful bladder syndrome, interstitial cystitis is a chronic bladder condition marked by persistent pain, pressure, and discomfort in the pelvic region. It also causes abnormal urinary frequency with relief after emptying the bladder, as well as pain during sex. Naturally, these symptoms can put quite a damper on one’s quality of life, making finding an effective treatment critical.
Though some reports suggest that painful bladder syndrome may affect up to 12 million people, there is still no definitive treatment for the condition. This makes managing the pain frustrating and difficult for many patients. While the medical field has made some strides with treatment options, many people find that making lifestyle changes, such as dietary changes and relaxing exercises, can help.
What Causes Interstitial Cystitis or Painful Bladder Syndrome?
Medical experts still don’t know exactly what causes the condition, but some believe it’s related to a problem with the bladder tissue, inflammation, or an irritant within the urine. Experts say that the issue is also more closely linked with the musculoskeletal structure, spurring the change in name.
“The medical industry is moving away from (the term ‘interstitial cystitis’), with the preferred term being ‘painful bladder syndrome,’” says Doctor of Physical Therapy Heather Jeffcoat, owner of Femina Physical Therapy in Los Angeles. “The reason for the name change is that the majority of cases are thought to be less of a bladder issue, and more of a disorder with a strong musculoskeletal contribution.”
There are two main subtypes of interstitial cystitis. In less than 10 percent of cases, patients have areas of inflammation on the bladder wall, called Hunner’s ulcers, which cause more severe symptoms. In other cases, the pain is caused by glomerulations, or areas of bleeding in the bladder lining. The remainder of cases are thought to be caused by pelvic floor muscle dysfunction.
What is Pelvic Floor Dysfunction? Learn More Here

Treating Painful Bladder Syndrome with Pelvic Floor Therapy
There is no one-size-fits-all approach to treating interstitial cystitis. Treatment plans depend on the specific patient and their subtype. However, because so much of the condition is caused by pelvic floor dysfunction, doctor-guided physical therapy for the pelvic floor can help sufferers of interstitial cystitis.
What is pelvic floor therapy? This form of treatment involves specialized exercises targeted at strengthening or loosening the muscles within the pelvic floor. In the case of painful bladder syndrome, the goal is to relax, or release, the tight pelvic floor muscles.
“(Treatment) will involve assessing and treating the muscles externally that attach at the pelvis,” says Dr. Rachel Gelman, owner of Pelvic Wellness & Physical Therapy in San Francisco. “If the patient consents, I will assess and treat the muscles internally, either vaginally or rectally. Treatment may include myofascial release, connective tissue manipulation and exercises to help teach the muscles how to move properly.”
Kegels and Interstitial Cystitis: Is It Safe?
Although Kegel exercises are a safe and effective form of therapy for similar conditions, including urinary incontinence, they aren’t recommended for sufferers of interstitial cystitis. This is because the primary purpose of Kegels is to tighten the muscles, which could worsen pain.
“If our muscles are contracting all the time, then they are not spending enough time in a relaxed, softened state,” says Dr. Jeffcoat. “If you continually contract, then your muscles will become short and tight over time. In the pelvic floor, this can lead to nerve impingement, nerve sensitivity, pain and additional muscle guarding around this pain, exacerbating the pain cycle.”
That doesn’t mean all self-guided exercises are off the table. The exercises listed below, as well as the use of a medical dilator or therapeutic pelvic massager (such as a TheraWand), can help patients practice internal release techniques, but they should be prescribed by a physical therapist.
Exercises for Relief from Painful Bladder Syndrome
It is also possible to release the muscle tension causing painful bladder syndrome with exercise at home. Healthy organs require plenty of blood flow, flexibility and strength, and the bladder is no different. Aim for low-impact exercises that help relax the pelvic floor muscles, such as those listed below.
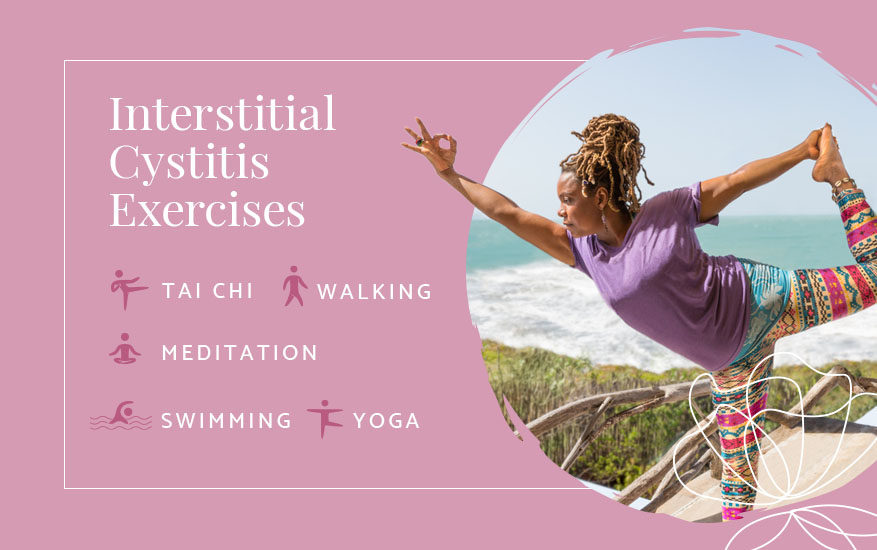
- Yoga — Dr. Jeffcoat recommends yoga for the pelvic floor to help relax the pelvic floor muscles. Two helpful poses are happy baby and child’s pose, both of which draw attention to the hip and help open the pelvis in a relaxed state. A yoga bolster or pillow can be useful in helping you stay comfortable while focusing on the pelvic floor during yoga.
- Meditation — Meditation on its own, as well as deep breathing during yoga practice, can help you relax tense muscles. “Deep breathing that includes lateral expansion of your ribcage — and visualization that as you inhale, your lungs fill with air — can create a feeling of heaviness and dropping of your pelvic floor muscles,” says Dr. Jeffcoat.
Discover How to Connect Your Pelvic Floor and Breathing
- Tai Chi — The traditional Chinese martial art of tai chi is touted as a gentle way to reduce muscle tension, increase flexibility and fight anxiety. Slow, measured movements can help encourage circulation and improve posture, which can help support the muscles that support the pelvic organs and prevent pain.
- Walking — Walking is another low-impact exercise that can boost circulation and provide muscle tension relief. The key is to make sure you’re walking at a slower pace and avoiding too much impact in the pelvic region.
- Swimming — Swimming is a gentle, low-impact exercise that can get the blood flowing to the pelvic muscles and organs. However, it’s important to note that some pool chemicals can worsen symptoms, so it may be best to avoid chlorine pools.

It’s important to speak to your doctor about taking on new exercises, as certain movements can tighten the muscles in the pelvic floor, which can contribute to additional pain and discomfort. If your symptoms persist or you notice lingering pelvic pain after exercise, it may be time to speak to your doctor and pursue more advanced treatment options.
Painful bladder syndrome is one of the most frustrating bladder conditions, but treating it with lifestyle changes such as exercise and seeking medical intervention can help you get back to living your best life free of pain and discomfort.
Image Credits
LightField Studios/Shutterstock.com
Drazen Zigic/Shutterstock.com
Pixel Prose Images/Shutterstock.com
karpenko_ilia/Shutterstock.com
LightField Studios/Shutterstock.com
Photographee.eu/Shutterstock.com